Released:3/14/2012 11:45 PM EDT
Embargo expired: 3/28/2012 7:30 PM EDT
Source:American Chemical Society (ACS)
EMBARGOED FOR RELEASE: Wednesday, March 28, 2012, 7:30 p.m. Eastern Time
Note to journalists: Please report that this research was presented at a meeting of the American Chemical Society
A press conference on this topic will be held at 2:15 p.m. Eastern Time, March 28, 2012, in the ACS Press Center, Room 15A, in the San Diego Convention Center. Reporters can attend in person or access live audio and video of the event and ask questions at www.ustream.tv/channel/acslive.
Newswise — SAN DIEGO, March 28, 2012 — If eccentric candy-maker Willy Wonka could leap from the pages of Roald Dahl’s classic, Charlie and the Chocolate Factory, and walk these streets, he might make a bee-line for a festival of cocoa and chocolate on the menu today at the 243rd National Meeting & Exposition of the American Chemical Society (ACS).
As the world’s largest scientific society, ACS is hosting a celebration of scientific discoveries about the food that could lay claim to being the world’s favorite treat, comfort food and indulgence. The ACS symposium, titled “Cocoa: Science and Technology,” features 18 reports from international experts on the key ingredient in chocolate — cocoa — and the emerging health benefits and other aspects of the food that has delighted people for almost 2,000 years.
“Chocolate is one of the foods with the greatest appeal to the general population,” said Sunil Kochhar, Ph.D., one of the symposium participants. “The luscious aroma, taste and textures of chocolate have delighted the senses of people in many parts of the world for centuries and make it a well-known comfort food.”
Kochhar, who is with the Nestlé Research Center in Lausanne, Switzerland, is noted for landmark research that is helping to establish chocolate’s potential health benefits. He described one study, for instance, published in the Journal of Proteome Research, one of ACS’s 41 peer-reviewed scientific journals, detailing the biochemical basis for chocolate’s reputation as a comfort food. The study, which included 30 healthy adults, found that eating about an ounce and a half of dark chocolate per day reduced levels of stress hormones and other indicators of emotional anxiety in people who felt stressed-out.
“The flavonoids and other ingredients in chocolate with beneficial health effects originate in cocoa,” Kochhar explained. “In making chocolate, cocoa seeds undergo natural fermentation before being processed into key ingredients for making chocolate — namely cocoa fat and cocoa powder.”
Among other presentations at the symposium, scientists reported:
- How the introduction of new varieties of the cacao tree that resist “witch’s broom,” a fungal disease that has decimated some crops, may affect the taste of cocoa and chocolate.
- That chocolate may be useful in treating of diseases involving disorders of the trigeminal nerve, including migraine and temporomandibular joint (TMJ) disorder. The study found evidence that cocoa contains biologically active ingredients that soothe the nerve’s excitability, a probable cause of these disorders.
- Findings about the biological basis of chocolate’s anti-inflammatory effects. Its rich content of polyphenols inhibit secretion of certain enzymes into the small intestine that cause inflammation.
- How chocolate may be helpful in fighting cardiovascular problems for individuals with type 2 diabetes. Flavonoids in the chocolate strengthen mitochondria, the powerhouse of body cells, which are in a weakened condition in patients with cardiovascular problems.
- On chocolate and high blood pressure. They found that flavonoids in chocolate lower blood pressure and thus might help in reducing heart disease risks.
- A cocoa-rich diet may reduce the risk of colon cancer by preventing undesirable changes in the cells or destroying cells that form precancerous lesions.
- That epicatechin, a beneficial antioxidant especially rich in dark chocolate, strengthens cell membranes and offers protection from some forms of cardiovascular disease.
- Feeding chocolate to animals in laboratory experiments helped protect their livers from damage that can lead to liver disease.
- Chocolate consumption may be especially beneficial for cigarette smokers. Polyphenols in the dark chocolate act on blood platelets to prevent clot formation.
The American Chemical Society is a non-profit organization chartered by the U.S. Congress. With more than 164,000 members, ACS is the world’s largest scientific society and a global leader in providing access to chemistry-related research through its multiple databases, peer-reviewed journals and scientific conferences. Its main offices are in Washington, D.C., and Columbus, Ohio.
To automatically receive news releases from the American Chemical Society contact newsroom@acs.org.
# # #
Selected abstracts from the symposium “Cocoa: Science and Technology” follow.
Abstracts
Cocoa and chocolate: The science of delightSunil Kochhar1, Nestle Research Center, P O Box 44, Lausanne-26, Vaud, Switzerland , 412 178 49336, sunil.kochhar@rdls.nestle.com
Chocolate is one of the foods with the greatest appeal to the general population. The attractive tastes and textures of chocolate and chocolate products delight the senses and make it a well-known comfort food. Cocoa seeds undergo natural fermentation before they are turned into a key ingredient for chocolate making namely cocoa fat and cocoa powder. The latter is indeed rich source of peptides and flavonoids, and produces the delectable taste and aroma of chocolate after roasting. In spite of a large body of literature on the cocoa flavor, there are very few studies devoted to the role of proteins/peptides in the flavor development of cocoa or chocolate. Cocoa storage proteins, which makes up to 10-15 % (w/w) dry weight, is made up of four predominant proteins of apparent molecular weight 14.5-, 31- and 47-kDa and 21-kDa representing 95 % (w/w) of total protein. We developed an in-vitro fermentation process of cocoa beans, mimicking the natural fermentation and identified a number short-chain peptides originating from storage proteins that are the key cocoa/chocolate flavor precursors. The presentation will cover the characterization of proteins and peptides and flavor precursors. Additionally, results from a recent study employing metabolomics approach to study the possible metabolic signatures linked to the regular intake of dark chocolate in healthy subjects will be presented. In summary, metabolic profiles of plasma and urine samples when combined with multivariate statistics show discrimination of subjects according to their chocolate liking as given by the scoring to the questionnaire on chocolate consumption. The class separation using plasma metabolic profiles was present even from samples collected before the chocolate intake, supporting most likely the occurrence of metabolic imprint or memory independent of the chocolate intake. Results indicate that subjects who do not like chocolate harbour statistically different lipoprotein profile in the postprandial phase.
Labels on chocolate bars: An accurate number for consumers to determine relative antioxidant contentJoe A Vinson1, Prof, PhD, University of Scranton, Department of Chemistry, Loyola Hall, University of Scranton, PA, 18510, United States , 570-941-7551, vinson@scranton.edu
There has been a dramatic increase in articles published about chocolate and health, especially related to heart disease and diabetes. Currently on the labels of many chocolate bars are % cacao solids (CS). But does this number have any relationship with the amount of polyphenol antioxidants in the product? Our group analyzed 31 commercial pure chocolate bars that have % CS on the label by Folin and FRAP. The catechin equivalents of the defatted extracts were corrected to determine polyphenols (µmol/g) in the chocolate bar. Foreign bars (milk and dark chocolate combined) have more antioxidants than domestic bars with the same % CS on the label. There is a significant linear relationship between % CS on the label and polyphenol content with both Folin and FRAP. Thus the consumer can know that 70% CS has about twice as much total antioxidants per serving as a bar with 35% CS.
Regulation of inflammatory proteins in trigeminal ganglion and trigeminal nucleus caudalis in response to cocoa enriched diets: Implications for migraine and TMJ disorderPaul L Durham1, Dr., PhD, 524 N Boonville, Springfield, MO, 65806, United States , 417-836-3026, pauldurham@missouristate.edu
The objective of our research was to investigate the cellular effects of a cocoa-enriched diet on neurons and glia in the trigeminal ganglia and trigeminal nucleus caudalis under basal conditions, and in response to acute or chronic inflammation. Sprague Dawley rats were fed a control diet or isocaloric diets enriched in cocoa for 14 days prior to injection of capsaicin or complete Freund's adjuvant (CFA). The stimulated expression of proteins associated with promoting and maintaining inflammatory and nociceptive responses were repressed in animals on a cocoa enriched diet. The inhibitory effects of cocoa are likely to be mediated via increased basal expression of the anti-inflammatory proteins MKP-1, MKP-3, and IL-10. Data from our study provide evidence that cocoa contains biologically active ingredients that modulate neuronal excitability, and thus, cocoa would be beneficial as a nutraceutical for the treatment of diseases involving trigeminal nerve activation such as migraine and TMJ disorder.
Alterations in skeletal muscle indicators of mitochondrial structure and biogenesis in patients with type 2 diabetes and heart failure: Effects of epicatechin rich cocoaFrancisco Villarreal1, Dr., MD, PhD, UCSD, Medicine, 9500 Gilman Dr., La Jolla, CA, 92093, United States , 858-534-3630, fvillarr@ucsd.edu
(-)-Epicatechin (Epi), a flavanol in cacao stimulates mitochondrial volume and cristae density and protein markers of skeletal muscle (SkM) mitochondrial biogenesis in mice. Type 2 diabetes mellitus (DM2) and heart failure (HF) are diseases associated with defects in SkM mitochondrial structure/function. A study was implemented to assess perturbations and to determine the effects of Epi-rich chocolate in SkM mitochondrial structure and mediators of biogenesis. Five patients with DM2 and stage II/III HF consumed dark chocolate containing ~100 mg of Epi/day for 3 months. We assessed changes in protein and/or activity levels of oxidative phosphorylation proteins, porin, mitofilin, nNOS, nitric oxide , cGMP, SIRT1, PGC1α, Tfam and, mitochondria volume and cristae abundance by electron microscopy from SkM. Apparent major losses in mitochondria structure and mediators of biogenesis were observed prior to treatment. Epi-rich cocoa increased protein and/or activity of these molecules as well as cristae abundance while not changing mitochondria volume density. Epi-rich cocoa treatment improves SkM mitochondrial structure and in an orchestrated manner, increases molecular markers of mitochondrial biogenesis resulting in enhanced cristae density. Future controlled studies are warranted using Epi-rich cocoa (or pure Epi) to translate improved mitochondrial structure into enhanced cardiac and/or SkM muscle function.
Dark chocolate inhibits platelet isoprostanes via nox2 down-regulation in smokersPasquale Pignatelli1, Md, PhD, Sapienza, University of Rome, Internal Medicine and Medical Specialities, Viale del Policlinico, Rome, Rm, Italy , 0039-6-4997-7777, pasquale.pignatelli@uniroma1.it
Dark chocolate receptors: Epicatechin-induced cardiac protection is dependent on delta-opioid receptor stimulation and altered membrane dynamics
Hemal H. Patel1,2, PhD, University of California, San Diego, Anesthesiology, VA San Diego Healthcare System, #125, 3350 La Jolla Village Dr., San Diego, CA, 92161, United States , 619-534-4906, hepatel@ucsd.edu Epicatechin, a dark chocolate flavonol/antioxidant, is linked to cardiovascular cytoprotection. Low-dose epicatechin, with little antioxidant activity, is protective; however, the mechanism of this cytoprotection is unknown. We tested if epicatechin mediates cardiac protection via delta opioid receptor (DOR) activation and modulation of membrane ultrastructure. Myocardial infarct size was decreased in epicatechin-treated mice compared to controls, and this effect was blocked by a DOR antagonist. Epicatechin increased phosphorylation of Src, Akt, and IκBα and decreased expression of c-Jun NH(2)-terminal kinase expression and caspase-activated DNase. DOR attenuated these signaling effects. Lipid rafts are critical for cardiac protection. The effect of epicatechin on cardiac myocyte membrane dynamics was examined with electron paramagnetic resonance (EPR) spectroscopy. Epicatechin increased membrane order parameter (decreased membrane fluidity) when compared to vehicle treated myocytes, an effect blocked by naloxone. In conclusion, epicatechin alters membrane dynamics and acts via DOR to produce cardiac protection from ischemia-reperfusion injury.
Systemic absorption and metabolism of proanthocyanidins in pigs
Hans-Ulrich Humpf1, Prof. Dr., University of Muenster, Institute of Food Chemistry, Corrensstr. 45, Muenster, NRW, 48149, Germany , +49 251 83 33391, humpf@uni-muenster.de
Cocoa, blood pressure and cardiovascular risk
Davide Grassi1, Dr, MD, PhD, University of L'Aquila, Internal Medicine and Public Hear, Viale S. Salvatore, Building Delta 6, L'Aquila, Italia, 67100, Italy , 0039 0862 434749, 0039 0862 434749, davide.grassi@cc.univaq.it Flavonoids from cocoa might exert some beneficial vascular effects and reduce the risk of cardiovascular morbidity and mortality. We observed that flavanol-rich but not flavanol-free chocolate administration was able to significantly lower both SBP and DBP in healthy subjects and in hypertensive patients with and without glucose intolerance. Further, flavanol-rich chocolate administration significantly improved nitric oxide-dependent flow-mediated dilation (FMD). Accordingly, different meta-analysis, on the effectiveness of flavonoid-rich foods on cardiovascular disease, reported that chocolate and cocoa intake significantly reduced SBP (-5.88 mmHg) and DBP (-3.30 mmHg). The antihypertensive responses observed support the inclusion of moderate amounts of flavanol-rich cocoa in the daily diet to potentially delay the onset of hypertension or ameliorate its control. Practicability of cocoa products as part of a long-term treatment for hypertension has yet to be completely explained. Further investigation on the dose-dependent and long-term effects of cocoa products should clarify these critical points.
Storage induced changes in lipid polymorphism in dark chocolate
Nicki J Engeseth1, Professor, Ph.D., University of Illinois, Food Science & Human Nutrition, 905 S. Goodwin, 208 Bevier, Urbana, IL, 61801, United States , 217-244-6788, engeseth@illinois.edu Chocolate is cocoa mass and sugar suspended in a cocoa butter matrix. Cocoa butter can crystallize in six structures, called polymorphs. Triglycerides reorganize to polymorph VI during long-term storage. Structural changes occur that are magnified with improper storage. Impact of storage conditions on polymorph transition and relationship to perception of chocolate flavor and texture were studied. Long term storage significantly impacts polymorph transition and flavor and texture of chocolate. Rate of polymorphic transition is often exacerbated by temperature cycling, typically used in research. Temperature cycling using different cycling regimes was conducted. Key differences between regimes revealed issues related to emulsification, leading to chocolate formulation with 3 emulsifiers. Chocolate formulated with these emulsifiers was subject to temperature cycling and long term storage. Key differences between emulsifiers and conditions will be highlighted. Future studies are aimed at compositional and structural information about triglycerides with different emulsifiers and use of novel processing strategies.
Cocoa flavonoids and effects on cardiovascular risk factors: Meta-analysis of randomized controlled trials
Eric L Ding1, PhD, Harvard Medical School, Brigham & Women's Hospital, Harvard School of Public Health, 655 Huntington Ave, Building 2, Department of Nutrition, Boston, Massachusetts, 02115, United States , 617-466-9626, eding@jhu.edu A growing body of evidence suggests that the consumption of foods rich in polyphenolic compounds—particularly cocoa—may have cardioprotective effects. No review, however, has yet examined the effect of flavonoid-rich cocoa on all major cardiovascular risk factors or has examined potential dose-response relationships for these effects. A systematic review and meta-analysis of randomized, controlled trials was performed to evaluate the effect of flavonoid-rich cocoa (FRC) on cardiovascular risk factors and to assess a dose-response relationship. Inclusion and exclusion criteria, as well as dependent and independent variables, were determined a priori. Data were collected for: blood pressure, pulse, total cholesterol, HDL cholesterol, LDL cholesterol, triglycerides, BMI, C-reactive protein, flow-mediated vascular dilation (FMD), fasting glucose, fasting insulin, serum isoprostane, and insulin sensitivity/resistance indices. Twenty-four papers, with 1106 participants, met criteria for final analysis. In response to FRC consumption, systolic blood pressure decreased by 1.63 mmHg (p=0.033), LDL cholesterol decreased by 0.077 mmol/L (p=0.038), and HDL cholesterol increased by 0.046 mmol/L (p=0.037), while total cholesterol, triglyceride, and CRP remained the same. Moreover, insulin resistance decreased (HOMA-IR: –0.94 points, p<0.001), while FMD increased (1.53%, p<0.001). A non-linear dose-response relationship was found between FRC and FMD (p=0.004), with maximum effect observed at a flavonoid dose of 500mg/day; a similar relationship may exist with HDL cholesterol levels (p=0.06). FRC consumption significantly improves blood pressure, insulin resistance, lipid profiles, and FMD. These short-term benefits warrant larger long-term investigations into the cardioprotective role of flavonoid-rich cocoa.
Dietary-feeding of cocoa prevents colonic preneoplastic lesions in azoxymethane-treated rats
Maria Angeles Martin1, ICTAN-CSIC, Department of Metabolism of Nutrition, C/ Jose Antonio Novais, 10, Madrid, Madrid, Spain , +34 915445607, amartina@ictan.csic.es Cocoa is a rich source of bioactive compounds with potential chemopreventive ability but up to date its effectiveness in animal models of colon carcinogenesis has not been addressed. Herein, we have used the well-defined azoxymethane (AOM)-induced colon cancer model in rats to investigate the ability of a cocoa enriched diet in preventing the early phase of chemically induced colorectal cancer. Our results showed that cocoa feeding significantly reduced AOM-induced colonic aberrant crypt foci formation and crypt multiplicity. Oxidative imbalance in colon tissues seems to be prevented by cocoa as indicated by reduced oxidation markers levels and increased enzymatic and non-enzymatic endogenous defences. Cocoa-rich diet also decreased the levels of proliferative and proinflammatory markers and induced pro-apoptotic effects. These findings provide evidences that a cocoa-rich diet may inhibit the early stage of colon carcinogenesis probably by preventing oxidative stress and cell proliferation and by inducing apoptosis.
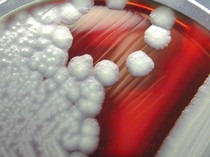
Unraveling the cocoa bean fermentation process opens new perspectives for chocolate production
Luc De Vuyst1, Prof. Dr. ir., PhD, Vrije Universiteit Brussel, Research Group of Industrial Microbiology and Food Biotechnology, Pleinlaan 2, Brussels, Belgium, B-1050, Belgium , +32-2-6293245, ldvuyst@vub.ac.be Cocoa fermentations are still carried out spontaneously. Once cocoa pods are opened, cocoa pulp-bean mass is inoculated by surrounding microbiota, which develop fast and selectively and ferment it for six days. A correct succession of microbial activities guarantees a successful fermentation process. Investigations of this process in several countries unraveled that always the same species of yeast, lactic acid bacteria, and acetic acid bacteria dominate the fermentation, independent of fermentation method and cocoa population, provided that good agricultural, fermentation and drying practices are applied. Several strains were tested in appropriate cocoa pulp simulation media to unravel their functional roles as well as in plastic vessels containing fresh cocoa pulp-bean mass as to their capacity to dominate the cocoa fermentation process. This procedure allowed us to develop a starter culture composed of Saccharomyces cerevisiae, Lactobacillus fermentum, and Acetobacter pasteurianus to improve the cocoa fermentation process. Uniformly fermented cocoa beans were obtained after four days of fermentation resulting in chocolate with standard flavor profiles.
Functional foods and food security: Cocoa mass and chocolates produced from "Witch Broom Disease” resistant cultivars of Brazil
Leonardo Fonseca Maciel1, Federa University of Bahia, Department of Bromatological Analysis, Rua Barão de Jeremoabo S/N Campus Universitário de Ondina, Faculdade de Farmácia, Ondina, Salvador, Bahia, 40170115, Brazil , 557132836970, lfmaciel@ufba.br The chocolate flavor is composed by many compounds whose formation depends on the genetic background and environment where cocoa is grown, as well as processing operations that begin on the farm and continue in the industries that process cocoa and chocolate. Cocoa production in Brazil suffered a sharp decline in the last two decades, due to a disease knowing as “witch broom disease” (Moniliophtora perniciosa). Trying to overcome this problem, cultivars resistant to fungus were obtained. Thus this study was carried out to evaluate the antioxidant capacity, phenolic compounds profile and mycotoxins (aflatoxin and ochratoxin) content from new cacao cultivars resistant to "witch broom disease” that were monitored during fermentation. Fruits of the new cocoa cultivars (SR162 and PH16), both resistant to “witch broom disease”, were studied and compared to conventional cocoa.
Cocoa-rich diet attenuates N-nitrosodiethylamine-induced liver injury in rats
Sonia Ramos1, ICTAN-CSIC, Department of Metabolism and Nutrition, Jose Antonio Novais 10, Madrid, Madrid, 28040, Spain , +34915492300, s.ramos@ictan.csic.es Cocoa has increasingly attracted attention due to its biological properties. The objective was to investigate the effects of cocoa feeding against N-nitrosodiethylamine (DEN)-induced liver injury in rats. Male rats were divided into five groups. Groups 1 and 2 were fed with standard and cocoa diet, respectively. Groups 3 and 4 were injected with DEN at 2 and 4 weeks, and fed with standard and cocoa diet, respectively. Group 5 was treated with DEN, received the standard diet for 4 weeks and then it was replaced by the cocoa-diet. The cocoa-rich diet prevented the reduction of hepatic glutathione concentration and catalase and GPx activities in DEN-injected rats, and diminished protein carbonyl content, caspase-3 activity, p-AKT and p-JNK levels, and increased GST activity. Cocoa administration did not abrogate the DEN-induced body weight loss, the increased levels of hepatic-specific enzymes and LDH. These results suggested that cocoa-rich diet attenuates the DEN-induced liver injury.